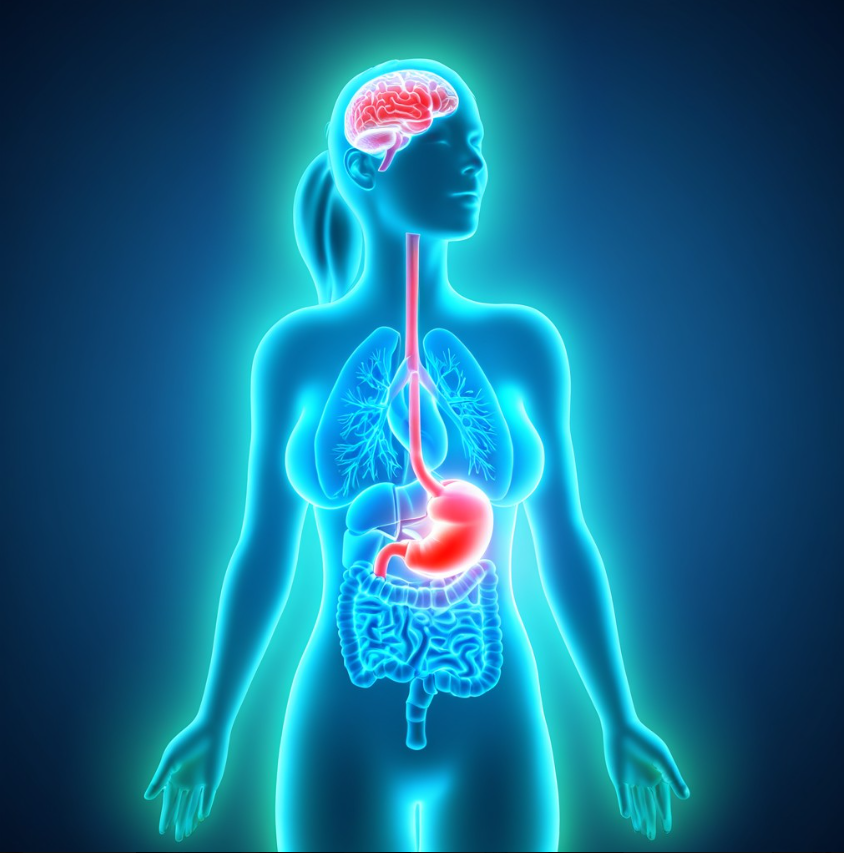
Introduction: Stress Is a Major, Overlooked Driver of Acid Reflux
Most people think their reflux comes from food alone. But for many individuals, stress is the true underlying trigger. Emotional pressure—whether from work, relationships, finances, or personal challenges—can activate the nervous system in ways that directly affect the throat, esophagus, stomach, and breathing.
At the Reflux Summit, we emphasize a whole-body understanding of reflux. Stress management is not “optional”—it’s an essential part of healing.
Why Stress Is a Major, Overlooked Driver of Acid Reflux
Most people think their reflux is caused by food alone. But for many, emotional stress is the real trigger—quietly influencing digestion, breathing, swallowing, and the esophageal valve.
Stress reshapes how the digestive system functions, often without the person feeling “stressed” in the traditional sense.
How Stress Affects Digestion and Reflux
Stress is not only emotional. It includes any event or feeling that disrupts your internal balance:
-
constant pressure or multitasking
-
emotional tension or conflict
-
worry, fear, or overthinking
-
grief or major life changes
-
burnout and chronic fatigue
These states activate the body’s stress response, which reduces digestive efficiency and increases reflux risk.
The Vagus Nerve: The Mind–Body Link Behind Stress-Driven Reflux
The vagus nerve is the primary communication channel between the brain and digestive system.
What the vagus nerve controls
-
throat and swallowing
-
the esophageal valve (LES)
-
stomach acid regulation
-
stomach emptying
-
intestinal movement
-
breathing patterns
-
heart rate and stress response
How stress disrupts vagus nerve function
When activated by emotional stress, the vagus nerve can:
-
weaken the esophageal valve
-
slow stomach emptying
-
increase pressure in the stomach
-
heighten esophageal sensitivity
-
trigger nausea or regurgitation
-
create throat tightness or shortness of breath
This is why reflux flares during arguments, stressful days, or emotionally heavy periods.
How Stress Makes Acid Reflux Worse
Weakened LES Function
Stress hormones can reduce the tone of the lower esophageal sphincter, allowing acid and stomach contents to flow upward.
Slowed Stomach Emptying
During “fight or flight,” digestion shuts down, causing food to sit longer in the stomach and increase reflux pressure.
Increased Sensitivity to Symptoms
Stress heightens nerve sensitivity, making mild reflux feel more intense or painful.
Vagus Nerve Overactivation
Strong emotional triggers can cause vagus-driven reactions such as chest tightness, shortness of breath, or a lump-in-throat feeling—often mistaken for severe reflux.
Signs Your Reflux Is Stress-Related
You may be experiencing stress-induced reflux if:
-
symptoms flare during emotional conversations
-
reflux happens even with “safe” foods
-
you feel chest or throat tightness under stress
-
flare-ups occur during big life transitions
-
symptoms calm down when you walk or relax
-
nighttime reflux appears during stressful periods
These patterns signal nervous-system involvement rather than dietary triggers.
Practical Ways to Reduce Stress-Driven Reflux
You don’t need complicated protocols—just consistent habits that calm the nervous system.
Focused Activities That Interrupt Overthinking
Choose activities that require attention and pull you out of your thoughts:
-
sports or movement activities
-
crafting, painting, or music
-
photography, nature observing, or birdwatching
-
puzzles, games, or brain challenges
-
weekly creative classes
The key is focus, not perfection.
One Weekly Activity That Connects You With Others
Human connection reduces stress hormones and improves vagal regulation.
Examples include:
-
book clubs
-
community groups
-
dance or fitness classes
-
volunteer activities
-
creative workshops
Choose something enjoyable and consistent.
A Simple 15–30 Minute Daily Walk
Walking calms the nervous system and gently stimulates digestion.
You can walk:
-
outdoors
-
on a treadmill
-
inside a mall
-
with a friend or pet
-
while listening to music or a podcast
Daily walking helps regulate breathing, digestion, and vagal tone.
When to Seek Professional Evaluation
Consider seeing a reflux specialist if:
-
symptoms persist despite stress management
-
you experience chronic throat symptoms
-
you have trouble swallowing
-
nighttime reflux becomes frequent
-
reflux affects your voice or breathing
-
symptoms last for months without improvement
A professional can determine whether symptoms come from acid, pepsin, motility issues, or nervous-system imbalance.
Final Thoughts: Stress Management Is Essential for Reflux Relief
Diet is important, but food isn’t the whole story. Stress has a powerful influence on the digestive system—often equal to or greater than dietary triggers.
By supporting your nervous system with consistent calming practices, many people experience major improvements in reflux symptoms.
Reflux healing involves both what you eat and how you live, breathe, and respond to stress.